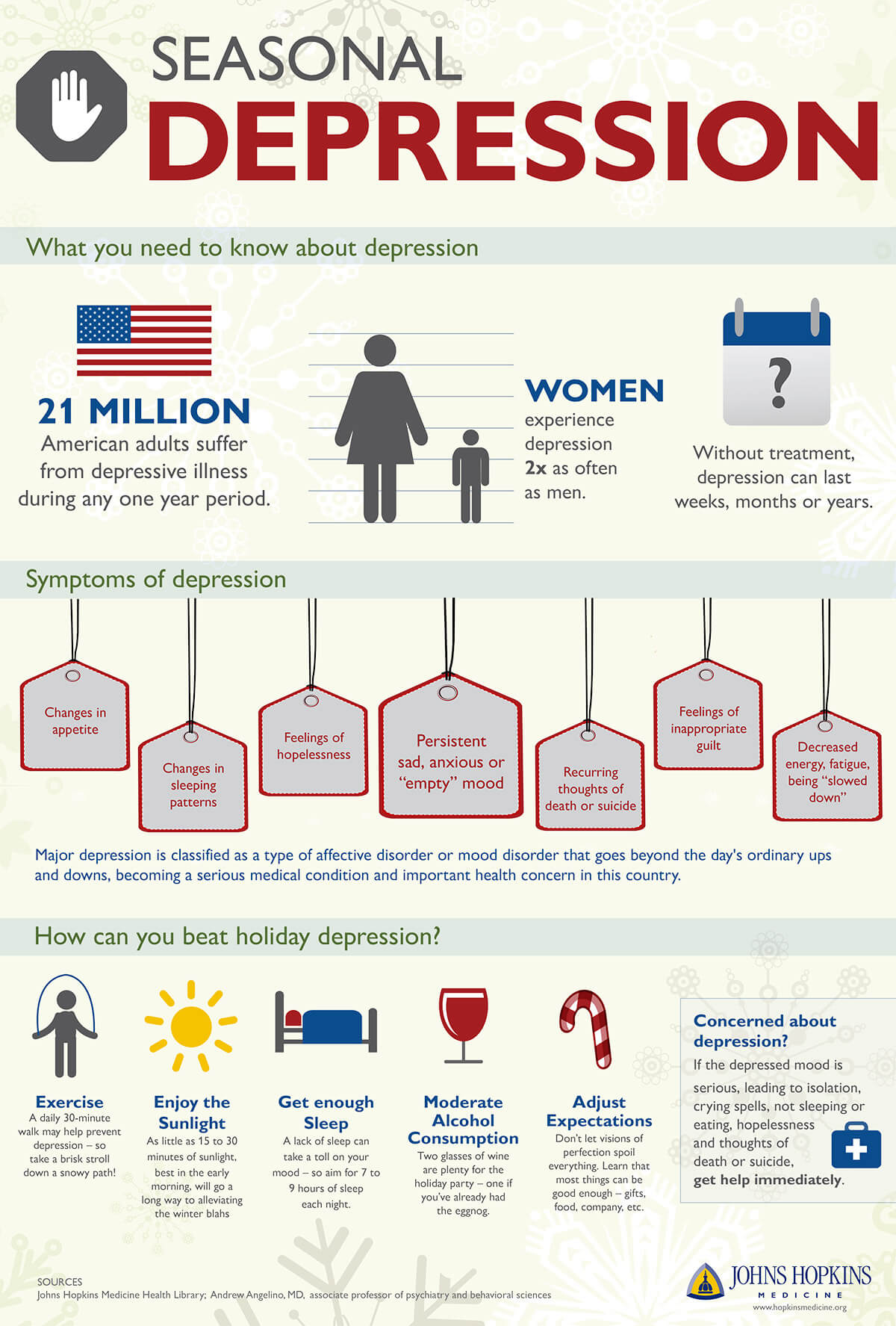
Seasonal affective disorder (SAD) is a type of depression linked to a lack of sunlight or changing seasons. It’s similar to the ‘winter blues’ but with more severe symptoms. People with SAD experience major depression during a specific time, usually winter. Symptoms often begin in the fall and continue through winter due to shorter days and colder weather.
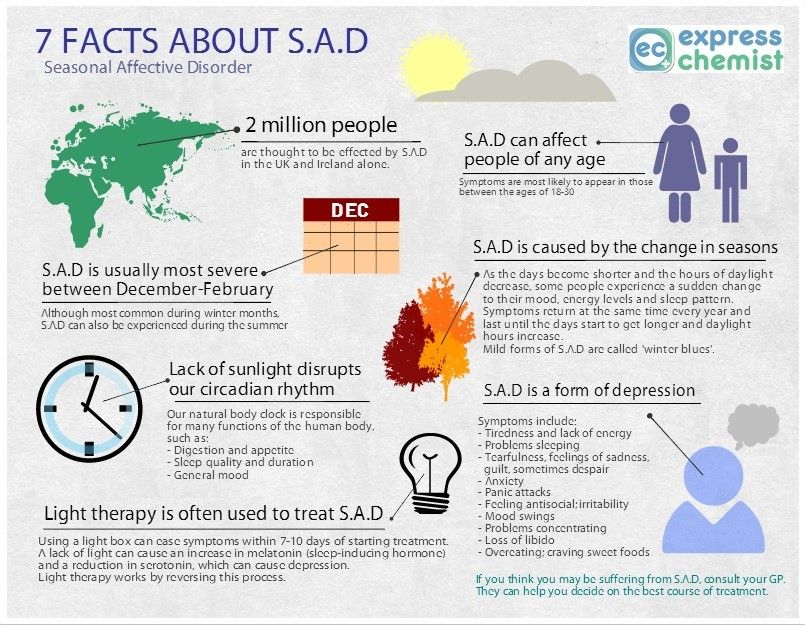
You may feel low on energy, sleep more, eat more, and have mood swings. However, when spring and summer come with longer days and warmer temperatures, your energy returns, and you feel happier. Sometimes, SAD can occur in spring or early summer and go away in fall or winter.

It can be tough, especially since Seasonal Affective Disorder (SAD) is connected to insufficient light exposure. For those affected, the gloomy, cloudy days or even being stuck in windowless offices and basement apartments can lead to feelings of sadness and depression, no matter the season.
Signs You Might Be Dealing with Seasonal Affective Disorder:
- Feeling down for pretty much the whole day, almost every day.
- Losing interest in the stuff you used to love doing.
- Feeling super low on energy and just kinda dragging around.
- Struggling with napping way too much
- Dealing with those pesky carb cravings, munching too much, and packing on the pounds.
- Struggling to focus
- Feeling down, like you have no worth, or just feeling guilty
- Having thoughts of not wanting to live
Feeling sad is totally normal, and we all go through it now and then. But if you’re stuck in that funk for several days and it’s messing with your life—like you’re not motivated or finding joy in things you used to love—maybe it’s a good idea to chat with your doctor.
When to Seek Help
If you experience these symptoms, consult a healthcare provider for a proper diagnosis, as they can rule out other conditions.

Is There Hope for Treating SAD?
Yes, Seasonal Affective Disorder can be treated. Treatments include light therapy (phototherapy), where exposure to bright light helps to regulate sleep patterns and mood, psychotherapy which provides support and strategies to cope with the emotional challenges of the condition, and medications that may involve antidepressants to help balance mood chemicals in the brain. Additionally, lifestyle changes such as increased physical activity, a healthy diet, and establishing a consistent routine can also play a crucial role in alleviating symptoms. It is important for individuals to seek professional guidance to determine the most effective treatment combination for their specific needs.

Depression isn’t just about feeling sad or down in the dumps. It’s not a sign that you’re weak or something you can just shake off. If you think you might be dealing with depression, talk to a healthcare professional as soon as you can. Left untreated, depression can drag on for weeks, months, or even years, but the good news is that a lot of people do well with medication, therapy, or a mix of both. Most people with clinical depression who reach out for help start feeling better in a few weeks.
Those Most Vulnerable to SAD
- Women are diagnosed with SAD about four times more often than men.
- Living further from the equator (e.g., New England, Alaska) increases risk due to less winter sunlight.
- SAD typically begins in early adulthood, often between ages 18 and 30.
- A history of depression, bipolar disorder, or family history of these conditions raises susceptibility.
- Certain gene variants related to circadian rhythms are linked to increased risk.
- Individuals with ADHD also show a higher likelihood of experiencing SAD.
Tips for Coping with SAD:
- Light Therapy: Use a bright light box (SAD lamp) daily, especially in the morning, to regulate your body clock.
- Natural Light: Maximize time outdoors, even on cloudy days, to absorb sunlight.
- Consistent Routine: Stick to regular sleep/wake times and mealtimes to stabilize your mood and energy.
- Exercise: Aim for 150 mins/week of moderate cardio; outdoor activity is best.
- Balanced Diet: Focus on lean proteins, Omega-3s, fruits (berries), veggies (dark leafy greens), and limit sugar.
- Vitamin D: Get levels checked by a doctor; supplements might be needed, but consult your doctor first.
- Therapy: Cognitive Behavioral Therapy (CBT) is effective for SAD; talk to a professional.
- Diary: Track symptoms and triggers to identify patterns
- Start Early: Begin preventive measures before symptoms get severe.
- Talk to Your Doctor: Get a proper diagnosis and discuss treatment options, including supplements.
Key Organizations & Resources:
- Anxiety and Depression Association of America (ADAA): Offers free, anonymous online support communities for anxiety, depression, trauma, and PTSD.
- National Alliance on Mental Illness (NAMI): Provides NAMI Connection (peer-led for mental health conditions) and family support groups, often with local chapters and virtual options.
- Depression and Bipolar Support Alliance (DBSA): Hosts online and in-person support groups for people with depression or bipolar disorder, plus groups for families.
- Mental Health America (MHA): Has a nationwide network of affiliates with community-specific programs and resources.
How to Find a Group:
- Online: Visit the websites of ADAA, NAMI, or DBSA to join virtual groups.
- Local: Search your state/county health department sites, or use NAMI’s “Find Your Local NAMI” tool.
- Professional Referral: Ask your doctor, therapist, or local hospital for recommendations.
What to Expect:
- Peer-Led: Groups are often run by trained individuals with lived experience.
- Structured: NAMI groups follow a model to ensure everyone gets a chance to speak.
- Safe & Welcoming: These are confidential spaces to share, learn coping skills, and build hope.

Leave a comment